 Should a quick bite between meals make us feel guilty? Or worse, make our teeth suffer a greater risk of cavities? Let’s avoid both those possibilities! We have several tooth-healthy
Read more
Should a quick bite between meals make us feel guilty? Or worse, make our teeth suffer a greater risk of cavities? Let’s avoid both those possibilities! We have several tooth-healthy
Read more
-
Snack Attack
posted: Apr. 23, 2024.
 Should a quick bite between meals make us feel guilty? Or worse, make our teeth suffer a greater risk of cavities? Let’s avoid both those possibilities! We have several tooth-healthy
Read more
Should a quick bite between meals make us feel guilty? Or worse, make our teeth suffer a greater risk of cavities? Let’s avoid both those possibilities! We have several tooth-healthy
Read more
-
Every Day is Earth Day
posted: Apr. 16, 2024.
 During the early days of the environmental awareness movement, those who demonstrated against pollution, toxic chemicals, and the general public health were known as hippies. The early 1970s were a
Read more
During the early days of the environmental awareness movement, those who demonstrated against pollution, toxic chemicals, and the general public health were known as hippies. The early 1970s were a
Read more
-
Sippy Cups
posted: Apr. 09, 2024.
 What a milestone! The transition from bottle to sippy cup is one of baby’s first steps toward toddler independence. And like all first journeys, some helpful guideposts come in handy.
Read more
What a milestone! The transition from bottle to sippy cup is one of baby’s first steps toward toddler independence. And like all first journeys, some helpful guideposts come in handy.
Read more
-
Do Spring Allergies Mean (B)Looming Dental Problems?
posted: Apr. 02, 2024.
 April showers bring May flowers, and May flowers bring . . . allergies. If you’re one of the millions of people who suffer from seasonal allergies, you might be suffering
Read more
April showers bring May flowers, and May flowers bring . . . allergies. If you’re one of the millions of people who suffer from seasonal allergies, you might be suffering
Read more
-
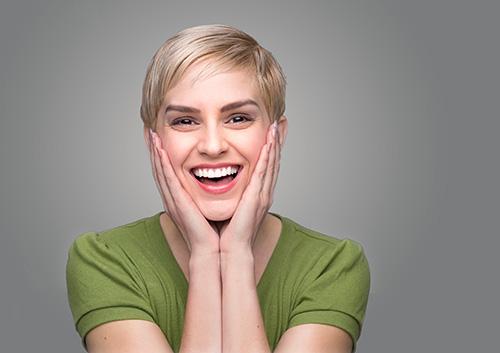
How do I overcome my dental anxiety?
posted: Mar. 26, 2024.
 Do you feel anxious before every dentist appointment? If the answer is yes, you are not alone—more than 75 percent of Americans feel anxious when visiting their dentist. Today, the
Read more
Do you feel anxious before every dentist appointment? If the answer is yes, you are not alone—more than 75 percent of Americans feel anxious when visiting their dentist. Today, the
Read more
-
The Link Between HPV and Oral Cancer
posted: Mar. 19, 2024.
 Cancer has become a common word, and it seems like there is new research about it every day. We know antioxidants are important. We know some cancers are more treatable
Read more
Cancer has become a common word, and it seems like there is new research about it every day. We know antioxidants are important. We know some cancers are more treatable
Read more
-
Going Green for St. Patrick’s Day?
posted: Mar. 12, 2024.
 Happily for all of us who like to celebrate with friends and family, there’s no need to be Irish to enjoy St. Patrick’s Day. Every March 17th, many of us
Read more
Happily for all of us who like to celebrate with friends and family, there’s no need to be Irish to enjoy St. Patrick’s Day. Every March 17th, many of us
Read more
-
Are your teeth ready for the big day?
posted: Mar. 05, 2024.
 Capturing the Moment
At Emerald Coast Family Dentistry we know that just about anyone who has taken on the challenge of planning her own wedding could tell you how important the
Read more
Capturing the Moment
At Emerald Coast Family Dentistry we know that just about anyone who has taken on the challenge of planning her own wedding could tell you how important the
Read more
-
Mamelons
posted: Feb. 27, 2024.
 Quick trivia question: define “mamelon.” Some kind of warm blooded animal? No, not a member of the mammal clan, but good guess. A fruit of the gourd family? Nope! There
Read more
Quick trivia question: define “mamelon.” Some kind of warm blooded animal? No, not a member of the mammal clan, but good guess. A fruit of the gourd family? Nope! There
Read more
-
Five Things You Didn't Know About Cavities
posted: Feb. 20, 2024.
 Most people know when they have a cavity—they can either see it on their tooth or... ouch! They can feel it! But there are certain things that many of our
Read more
Most people know when they have a cavity—they can either see it on their tooth or... ouch! They can feel it! But there are certain things that many of our
Read more
-
Team Dark Chocolate
posted: Feb. 13, 2024.
 Valentine’s Day is the holiday to celebrate all the treasured relationships in your life. It’s a time to honor love in all shapes and forms with cards, social gatherings, and
Read more
Valentine’s Day is the holiday to celebrate all the treasured relationships in your life. It’s a time to honor love in all shapes and forms with cards, social gatherings, and
Read more
-
February is Heart Month
posted: Feb. 06, 2024.
 The American Academy of Periodontology stresses the importance of good oral health since gum disease may be linked to heart disease and stroke. Thus far, no cause-and-effect relationship has been
Read more
The American Academy of Periodontology stresses the importance of good oral health since gum disease may be linked to heart disease and stroke. Thus far, no cause-and-effect relationship has been
Read more
-
Oral Health for the Young Adult
posted: Jan. 30, 2024.
 Young adults often have the reputation of not taking good care of themselves. You may feel invincible, and not realize how much your behaviors now can affect your health later
Read more
Young adults often have the reputation of not taking good care of themselves. You may feel invincible, and not realize how much your behaviors now can affect your health later
Read more
-
Is Charcoal Teeth Whitening Safe?
posted: Jan. 23, 2024.
 Health and beauty trends surface on the web every day, and it can be difficult to tell which ones are worth your time, or even safe, for that matter. Perhaps
Read more
Health and beauty trends surface on the web every day, and it can be difficult to tell which ones are worth your time, or even safe, for that matter. Perhaps
Read more
-
What is hand-foot-and-mouth disease?
posted: Jan. 16, 2024.
 Hand-foot-and-mouth disease, or HFMD, is a type of contagious viral illness that causes a rash in the mouth and on the hands and feet of infants and young children, and,
Read more
Hand-foot-and-mouth disease, or HFMD, is a type of contagious viral illness that causes a rash in the mouth and on the hands and feet of infants and young children, and,
Read more
Contact Us
Contact Us
Hours of Operation
Monday:
8:00 am-5:00 pm
Tuesday:
8:00 am-5:00 pm
Wednesday:
8:00 am-5:00 pm
Thursday:
8:00 am-5:00 pm
Friday:
Closed
Saturday:
Closed
Sunday:
Closed
